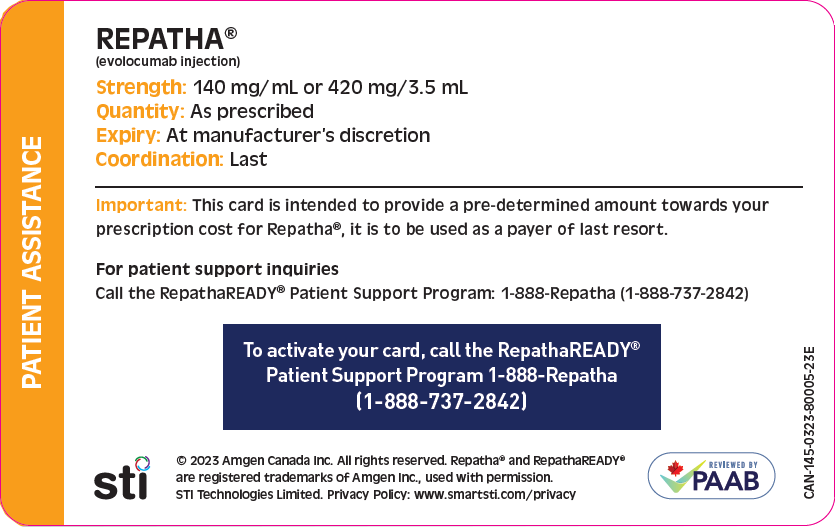
To assist your clinic in completing private insurance special authorization forms for your patients who have been prescribed Repatha®, the following suggestions and tips have been compiled. You may find these tips useful for filling in reimbursement criteria and history as requested, according to your individual patient’s diagnosis and treatment history.
Please ensure that the primary indication for treatment is specified:
- Adult patients with ASCVD: prevention of cardiovascular events: adjunct to diet and standard of care therapy to reduce risk of MI, stroke and coronary revascularization; or
- Primary hyperlipidemia including HeFH: reduction of elevated LDL-C. See below for Repatha® indications.
Forward completed special authorization forms to RepathaREADY®